In the vast tapestry of human health, certain conditions, lurking within the confines of our most vital organ, have long enticed the curiosity of medical researchers and mystified even the most seasoned clinicians. At the heart of this enigmatic realm lies a complex web of aberrant growths, covertly infiltrating the delicate landscape of the brain. These formidable adversaries, shrouded in mystery and untold potential, are commonly referred to as cerebral lesions.
Like enigmatic whispers in a labyrinth, the world of cerebral neoplasms beckons us to navigate its intricacies, to unravel the very essence of their existence. Within these cerebral potentialities await an abundance of puzzles yearning to be solved, their answers capable of revolutionizing the field of neurosurgery and offering new hope to countless individuals. But untangling the enigma of cerebral lesions demands not only scientific rigor but also the tenacity to delve into their shadowy depths.
Despite their seemingly sinister nature, cerebral lesions are an embodiment of biological complexity, infused with both enigmatic beauty and a myriad of possibilities. The emergent hallmark of deciphering these inexplicable clusters lies in understanding the intricate tapestry of genetic mutations, cellular dynamics, and physiological disruptions that give rise to these cerebral conundrums. Only then can we pave the way towards a future where the mysteries of these tumors are unraveled, and their impact on the human brain mitigated.
The Intricate World of Intracranial Neoplasms: Grasping the Fundamentals
Exploring the multifaceted realm residing within the confines of the human cranium, one encounters an intriguing dimension - the enigmatic domain of intracranial neoplasms. These complex entities, obscured by the complexity of cerebral anatomy and physiology, present an intricate puzzle that continuously challenges the scientific community. By delving into the fundamental aspects underlying these enigmatic growths, we strive to decipher their clandestine nature.
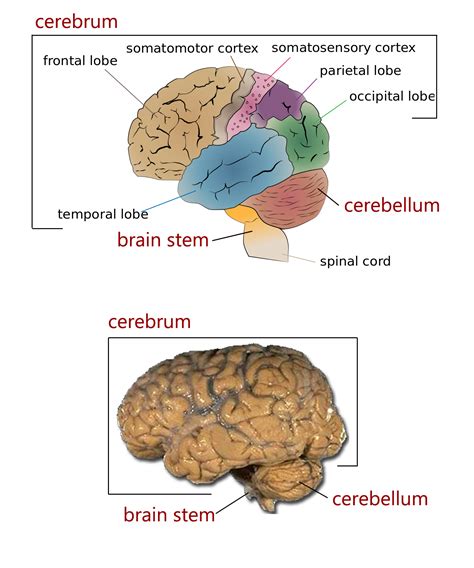
Embarking on our quest to understand the basic essence of intracranial neoplasms, it becomes essential to traverse the vast spectrum of intricacies they entail. Gaining insight into their molecular origins, genetic intricacies, and diverse anatomical locations, we unravel the intricate tapestry that interweaves the web of these perplexing entities. Through this exploration, we seek to grasp the essence of their growth patterns, distinguish their various types, and ultimately comprehend the effect they have on the surrounding cerebral structures.
- Origins of Intracranial Neoplasms:
- Genetic mutations and aberrations
- Molecular pathways and signaling networks
- Classification of Intracranial Neoplasms:
- Primary brain tumors
- Metastatic brain tumors
- Growth Patterns and Anatomical Locations:
- Infiltrating tumors
- Benign tumors
- Midline vs. hemispheric tumors
- Impact on Cerebral Structures:
- Compression and displacement
- Mass effect on adjacent tissues
- Neurological symptoms and deficits
By embracing the complexities surrounding intracranial neoplasms and contemplating the evolving scientific insights, we embark on a journey towards unraveling the mysteries that lie within the intricate world they inhabit. Through understanding their fundamental aspects, we pave the way for improved diagnostics, treatment strategies, and ultimately, enhanced patient outcomes.
Understanding the Diversity of Brain Tumors: Exploring the Spectrum of Benign and Malignant Forms
In the realm of neurological health, the intricacies surrounding brain tumors have long puzzled and fascinated scientists. Within this complex domain, brain tumors manifest in diverse forms, spanning a spectrum that includes both benign and malignant forms. This section aims to shed light on the distinct types of brain tumors, examining their varied characteristics and potential implications.
- Gliomas: Among the most prevalent types of brain tumors, gliomas arise from the glial cells that support and protect the neurons. As these tumors develop, they may take on different forms, including astrocytomas, oligodendrogliomas, and ependymomas.
- Meningiomas: Originating from the meninges, the protective membranes surrounding the brain and spinal cord, meningiomas are primarily benign tumors. However, their location within the skull can lead to problematic symptoms as they grow and compress surrounding structures.
- Pituitary adenomas: Deriving from the pituitary gland, these tumors typically fall under the benign category. Despite this, they can cause significant disruptions in hormone regulation due to their impact on the pituitary gland's normal functioning.
- Medulloblastomas: Primarily affecting children, medulloblastomas arise in the cerebellum, the part of the brain responsible for coordinating movement and balance. These malignant tumors necessitate specialized treatment approaches due to their unique characteristics and the vulnerable age group they typically affect.
- Metastatic brain tumors: Forming when cancer spreads from other parts of the body, metastatic brain tumors can encompass various cancer types. Their presence in the brain often indicates advanced stages of cancer and requires thorough diagnosis and individualized treatment plans.
As one delves into the realm of brain tumors, it becomes evident that these growths are not a homogenous entity but a complex array of distinctive types. Through understanding the specific characteristics, behaviors, and potential implications associated with distinct brain tumors, the medical community moves closer to unraveling the enigmatic nature of these conditions.
Beyond Genetics: Investigating the Risk Factors Associated with Brain Tumors
Understanding the factors that contribute to the development of brain tumors extends far beyond genetic influences. While genetics undoubtedly play a role, there are various other elements that come into play. By exploring these risk factors, we can gain a deeper understanding of the complexities surrounding brain tumor formation.
- Environmental Exposures: The environment we live in can introduce potential risk factors for brain tumors. Exposure to certain chemicals, radiation, or electromagnetic fields may contribute to the development of these tumors.
- Lifestyle Choices: Certain lifestyle factors have been linked to an increased risk of brain tumors. These may include smoking, excessive alcohol consumption, poor diet, lack of physical activity, and exposure to secondhand smoke.
- Occupational Hazards: Some occupations may expose individuals to higher levels of potential carcinogens, thus increasing the risk of brain tumors. These jobs range from agricultural work to industrial settings where exposure to harmful substances is prevalent.
- Preexisting Medical Conditions: Certain medical conditions, such as neurofibromatosis or Li-Fraumeni syndrome, have been associated with an elevated risk of developing brain tumors.
- Prior Radiation Therapy: Individuals who have undergone radiation treatment for other conditions, particularly at a young age, may have an increased risk of developing brain tumors later in life.
- Age and Gender: The risk of brain tumors can vary based on age and gender. Certain types of brain tumors are more common in specific age groups, while men and women may exhibit different susceptibilities to certain tumor types.
By delving into these diverse risk factors, researchers aim to unravel the complex web of influences that contribute to the development of brain tumors. Understanding the interplay between genetics, environmental exposures, lifestyle choices, and other factors is crucial in developing strategies for prevention and early detection.
Facing the Silent Enemy: Recognizing the Symptoms of Intracranial Masses
When it comes to intracranial masses, awareness of their symptoms is crucial for early detection and intervention. These silent adversaries, lurking within the intricate network of our central nervous system, present a formidable challenge in the battle for our well-being. Recognizing the subtle signs they may manifest can be the first step towards reclaiming control over our health.
Awareness of the warning signs is essential in identifying potential intracranial masses. Symptoms can vary depending on the size, location, and type of the tumor. They may arise from various physiological processes such as the expanding mass exerting pressure on surrounding structures, disruption of normal brain functions, or the release of certain substances by the tumor itself. While the effects can be diverse, it is imperative to stay vigilant and acknowledge any alterations in our physical or mental well-being.
It is crucial to pay attention to recurring headaches that are unresponsive to normal pain relief measures or display unique patterns in intensity, duration, or location. Cognitive changes, such as memory loss, difficulty concentrating, or sudden mood swings, should not be overlooked, as they may indicate the presence of an intracranial mass. Additionally, unexplained seizures, hearing or vision problems, and unsteadiness in coordination might warrant further investigation, as they could be potential red flags for the silent enemy.
An emphasis should also be placed on recognizing the subtler signs that may go unnoticed amidst the chaos of daily life. Fatigue, unexplained weight loss or gain, and changes in taste or smell perception could all indicate an underlying intracranial mass. In children, developmental delays, excessive irritability, or changes in behavior and sleep patterns may be indicative of a silent enemy silently invading their young minds.
Ultimately, vigilance, coupled with proactive communication with healthcare professionals, plays a pivotal role in recognizing the symptoms associated with intracranial masses. By remaining vigilant, we empower ourselves to identify potential threats and take necessary actions towards early diagnosis, personalized treatment, and the ultimate preservation of our well-being.
Connecting the Pieces: Identifying and Diagnosing Intriguing Cerebral Growths
In this section, we explore the intricate puzzle of detecting and diagnosing enigmatic formations within the human brain. Through a meticulous process guided by medical expertise and advanced technology, medical professionals endeavor to unravel the enigma that lies within these captivating abnormalities.
Assembling the medical jigsaw puzzle begins with a comprehensive evaluation of clinical symptoms exhibited by affected individuals. These diverse manifestations, which can vary widely, serve as invaluable clues that hint at the presence of these inscrutable formations. Subtle changes in behavior, cognitive functions, or sensory perception can often provide the first pieces of the puzzle for astute physicians.
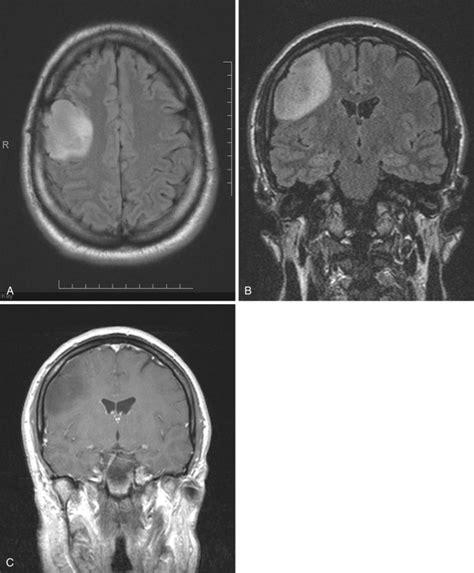
Utilizing cutting-edge imaging techniques, such as magnetic resonance imaging (MRI) and positron emission tomography (PET), medical practitioners are able to peer beneath the veil of the brain's intricate veil to expose the presence of these mysterious growths. This imagery is akin to a map, guiding physicians along the twisted paths and contours of the brain, allowing them to take note of any irregularities or hidden tumors.
Once potential trouble spots have been identified, medical professionals embark on an intricate process of analysis, which involves careful evaluation of tissue samples procured through biopsy. Examining these microscopic fragments under a microscope helps to paint a richer picture of the cellular composition, providing crucial insights into the nature and behavior of the tumors.
- Identifying the specific type of tumor is paramount, as it determines the course of treatment and prognosis for affected individuals. Certain tumors may be benign, remaining relatively stationary and unlikely to cause significant harm, while others may be malignant, exhibiting aggressive growth and potential for metastasis.
- Gaining a deeper understanding of the tumor's genetic and molecular makeup is also crucial. These delicate strands of information can illuminate the underlying mechanisms that drive tumor growth, potentially unveiling targets for tailored therapies.
- Collaboration among multidisciplinary teams of healthcare professionals plays a vital role in accurately diagnosing brain tumors. Expertise from neurosurgeons, radiologists, pathologists, and oncologists is crucial in piecing together the complex puzzle and ensuring the most effective treatment plan.
In conclusion, the journey of diagnosing brain tumors is akin to piecing together a captivating puzzle. Each symptom, medical image, and microscopic examination acts as a profound clue, gradually forming a comprehensive understanding of the enigma that resides within the intricacies of the human brain. The power of collaboration and cutting-edge technology empowers medical professionals to unlock these mysteries and pave the way for effective treatment and improved outcomes for those affected.
Treatment Options: Discovering Hope in the Battle Against Brain Tumors
In this section, we delve into the various strategies and techniques that offer potential avenues for combating tumors within the intricate neural structure. Exploring a range of possibilities, we seek to shed light on the diverse treatment options that hold promise in the ongoing battle against these formidable mass lesions.
Advancing the Frontiers: Future Breakthroughs in Research on Brain Tumors

In this section, we will explore the exciting avenues that lie ahead in our quest to uncover the enigmas surrounding tumors within the human brain. Groundbreaking discoveries and technological advancements are poised to reshape the future of brain tumor research, providing new avenues for diagnosis, treatment, and prevention.
1. Diving Deeper: Enhanced Imaging Techniques
- Advancements in imaging modalities such as magnetic resonance imaging (MRI) and positron emission tomography (PET) are revolutionizing our ability to visualize brain tumors with greater precision and accuracy.
- Novel imaging probes and contrast agents are being developed to specifically target tumor cells, allowing for earlier detection and more effective monitoring of treatment response.
- The integration of artificial intelligence and machine learning algorithms with imaging data promises to improve diagnostic accuracy and aid in the identification of genetic markers associated with different tumor types.
2. Unmasking the Biological Drivers: Genomic Profiling and Precision Medicine
- Advances in genomic profiling are shedding light on the complex molecular underpinnings of brain tumors, unraveling their distinct genetic alterations and identifying potential targets for personalized therapies.
- The emergence of precision medicine approaches, including targeted therapies and immunotherapies, offers new hope for improved treatment outcomes by tailoring interventions to the unique characteristics of individual patients.
- Collaborative efforts such as international consortia and data-sharing initiatives are facilitating the integration of large-scale genomic data, leading to a deeper understanding of tumor heterogeneity and paving the way for more effective treatment strategies.
3. Nanomedicine: Beyond the Blood-Brain Barrier
- The development of nanotechnology-based delivery systems holds immense promise for overcoming one of the greatest challenges in brain tumor treatment – the blood-brain barrier.
- Nanoparticles loaded with therapeutic agents can bypass this protective barrier, delivering drugs directly to tumor cells while minimizing systemic toxicity.
- Engineered nanoparticles are being utilized not only for drug delivery but also for targeted imaging, allowing for real-time monitoring of treatment response and the identification of potential therapeutic targets.
As we venture into the uncharted territories of brain tumor research, these future advances bring renewed hope for better diagnostics, treatments, and ultimately, improved patient outcomes. By combining innovative technologies, interdisciplinary collaborations, and a patient-centric approach, we are poised to make significant strides in our journey to conquer the mysteries of brain tumors.
FAQ
What are some common symptoms of brain tumors?
Common symptoms of brain tumors can include frequent headaches, seizures, changes in vision, difficulty speaking or understanding language, loss of coordination, and changes in mood or personality.
Can brain tumors be inherited?
While brain tumors can occur in individuals with a family history of the condition, they are generally not considered to be inherited. Most brain tumors develop sporadically, with no clear genetic cause.
What are the treatment options available for brain tumors?
Treatment options for brain tumors can vary depending on the type, size, and location of the tumor. They may include surgery, radiation therapy, chemotherapy, targeted therapy, and immunotherapy. The best treatment approach is determined on a case-by-case basis by a team of healthcare professionals.
Are all brain tumors cancerous?
No, not all brain tumors are cancerous. Brain tumors can be classified as either benign or malignant. Benign tumors are non-cancerous and generally have a better prognosis, while malignant tumors are cancerous and have the potential to spread to other parts of the body.



