Have you ever found yourself transported to a hazy world where the air feels thick, and your chest aches with a lingering discomfort? It is a realm where the body's complex machinery produces a peculiar substance, one that is often met with disdain and an inherent desire for its expulsion. This enigmatic creation, although disconcerting, is an essential bodily function that serves a vital purpose. We find ourselves delving into the realm of respiratory health, exploring the intricate dance between the environment and our bodies, and the resulting formation of dense phlegmatic secretions.
Embarking on this intriguing journey, we seek to unravel the myriad factors that contribute to the production of this viscid concoction. Our exploration takes us through the labyrinth of various irritants, lurking pathogens, and underlying medical conditions that act as catalysts for its formulation. From the embers of chest congestion to the residue of seasonal allergies, a panorama of possible causes awaits our investigation.
As we delve deeper into this murky domain, we encounter a complex concoction of symptoms that accompany the presence of thickened phlegm. A relentless cough, persistently blocked nasal passages, and a general feeling of heaviness underscore the discomfort experienced by those afflicted. This tangible manifestation of our body's intricate defense mechanisms is a potent clue, a signal that our respiratory system is working diligently to combat external aggressors and restore equilibrium.
Yet fear not, for science and nature have conspired to provide us with a range of effective remedies to counteract the presence of this thick substance that threatens our comfort and well-being. From age-old herbal concoctions to modern medicinal breakthroughs, there exists an arsenal of solutions to diffuse the discomfort rooted in excess mucus production. Armed with this knowledge, we empower ourselves to navigate through the realms of symptom relief and restore our respiratory sanctuaries to their optimal state of bliss.
Understanding the Essential Role of Phlegm in the Respiratory System
Exploring the Significance of Phlegm in Maintaining Respiratory Health
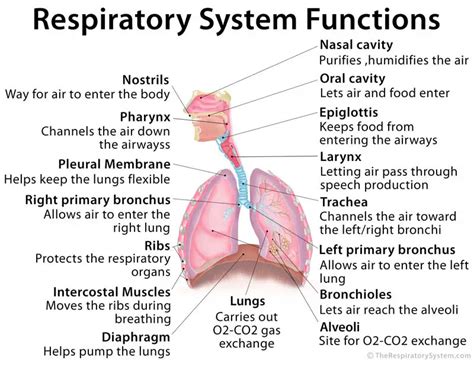
Phlegm, a viscous substance produced by the respiratory system, plays a vital role in maintaining the health and functionality of our lungs and airways. Although commonly associated with discomfort or illness, phlegm serves an important purpose as a defense mechanism against potential infections and foreign particles that enter the respiratory tract.
Understanding the Composition and Function of Phlegm
Composed of water, mucus, glycoproteins, and various immune cells, phlegm acts as a protective barrier in the respiratory system. It is responsible for trapping and expelling harmful substances such as bacteria, viruses, allergens, and irritants that we inhale daily. This helps prevent these harmful agents from infiltrating deeper into the lungs, causing more severe respiratory issues.
The Key Role of Phlegm in Clearing Respiratory Passages
Phlegm serves as a natural self-cleansing mechanism within our respiratory passages. When foreign particles or pathogens are detected in the airways, the body produces additional phlegm to help flush out these invaders. Cilia, tiny hair-like structures lining the airways, work in conjunction with the sticky nature of phlegm to facilitate the upward movement of mucus and trapped substances, effectively clearing the respiratory passages.
Phlegm's Diagnostic Value in Identifying Respiratory Conditions
The color, consistency, and quantity of phlegm can provide valuable insights into the presence and nature of respiratory conditions. Analyzing these characteristics can aid in the diagnosis and management of respiratory ailments including colds, bronchitis, pneumonia, and chronic obstructive pulmonary disease (COPD). It is important to note that monitoring phlegm alone should not substitute professional medical advice, but it can serve as an indicator for seeking appropriate healthcare.
Conclusion
Considering the essential role of phlegm in the respiratory system, it becomes evident that this sticky substance is not merely a nuisance, but rather a crucial component for maintaining lung health. Understanding how phlegm functions in capturing and clearing harmful particles, as well as its potential diagnostic value, highlights the significance of recognizing and appreciating the role it plays in our overall well-being.
Unveiling the Reasons Behind Excessively Produced Mucus
In this section, we will delve into the various factors that contribute to the overproduction of mucus in the body. This excessive mucus production can lead to discomfort and various health issues, making it important to understand the underlying causes.
Excessive mucus production can be influenced by a multitude of elements, such as environmental factors, lifestyle choices, and physiological conditions. Understanding these factors can help identify potential triggers and pave the way for effective management strategies.
- Environmental Factors: Certain environmental conditions, such as air pollution, allergens, and exposure to irritants like smoke or chemicals, can stimulate the body to produce additional mucus as a defense mechanism.
- Lifestyle Choices: Smoking, poor diet, lack of hydration, and sedentary lifestyle can all contribute to an increase in mucus production. Making healthier choices in these areas can play a crucial role in reducing excess mucus.
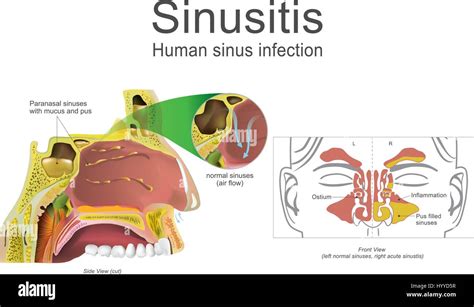
- Physiological Conditions: Certain medical conditions like allergies, respiratory infections, sinusitis, asthma, and postnasal drip can lead to excessive mucus production. Identifying and treating these conditions can help alleviate the symptoms associated with increased mucus production.
By understanding the causes of excessive phlegm production, individuals can take proactive measures to reduce its occurrence. This can involve making lifestyle changes, implementing preventive strategies, and seeking professional medical advice when necessary. However, it is important to note that each person's situation may vary, and it is always advisable to consult with a healthcare professional for personalized guidance.
Recognizing Common Signs of Thick Mucus
Introduction: This section aims to shed light on the typical indications that accompany the presence of dense phlegm. By understanding the symptoms associated with this condition, individuals can better identify and address potential respiratory issues.
1. Persistent Coughing: A frequent and prolonged cough can be a telltale sign of the presence of thick mucus in the airways. This symptom may accompany other respiratory conditions and can be further aggravated by certain triggers.
2. Difficulty Breathing: Thick phlegm can obstruct the respiratory pathways, leading to difficulty in breathing. Individuals may experience shortness of breath, wheezing, or a sensation of tightness in the chest. These symptoms may worsen during physical exertion or exposure to allergens.
3. Excessive Mucus Production: An increased quantity of mucus being produced is often indicative of thick phlegm. This excess mucus may be visible as yellow or greenish discharge, which can further contribute to respiratory congestion.
4. Throat Irritation and Soreness: The presence of thick phlegm in the throat can result in irritation and discomfort. Individuals may experience a persistent scratchy or ticklish sensation, which can lead to a sore throat.
5. Chest Congestion: Thick phlegm can contribute to a feeling of heaviness or congestion in the chest. This sensation may be accompanied by a rattling or gurgling sound while breathing.
6. Recurrent Infections: People experiencing frequent respiratory infections, such as sinusitis or bronchitis, may have an underlying issue with thick mucus production. This persistent problem can impede the body's ability to clear out pathogens, leading to recurrent infections.
By paying attention to these common symptoms, individuals can take proactive steps to identify and address any potential concerns related to thick phlegm. Seeking medical advice is essential for an accurate diagnosis and to determine the most suitable remedies or treatments.
Allergy-Induced Factors in the Formation of Mucus
Allergies play a significant role in the development of excessive mucus production within the respiratory system. When individuals are exposed to allergens, such as pollen, dust mites, or pet dander, their immune system reacts by releasing histamine, a compound that triggers an inflammatory response. This inflammation causes the blood vessels within the nasal passages and airways to dilate and become more permeable, leading to an influx of fluids and immune cells. As a result, the respiratory mucosa becomes swollen and produces an excessive amount of mucus to trap and eliminate the allergens.
Allergic Rhinitis:
One common manifestation of allergies that contributes to the formation of thick mucus is allergic rhinitis, also known as hay fever. This condition is characterized by persistent sneezing, nasal congestion, itching, and watery discharge from the nose. In response to airborne allergens, the body releases an increased amount of mucus, leading to a congested and stuffy sensation. As the body attempts to remove these irritants, the consistency of the mucus may become thicker and stickier.
Role of Immunoglobulin E (IgE):
Immunoglobulin E, or IgE, is an antibody produced by the immune system in response to allergens. When exposed to an allergen, the body produces IgE, which binds to mast cells and basophils. These cells are responsible for releasing histamine, cytokines, and other inflammatory mediators that initiate the allergic response. The release of these substances leads to vasodilation, increased mucus production, and infiltration of inflammatory cells in the respiratory mucosa, resulting in the formation of thick phlegm.
Environmental Allergens:
Various environmental factors can trigger allergies, leading to the production of thick phlegm. Common environmental allergens include pollen, mold spores, dust mites, and animal dander. When individuals with allergies come into contact with these substances, their immune system perceives them as foreign invaders and responds by releasing histamine and other chemicals. This immune response results in the secretion of excess mucus, which may become thick and difficult to expel.
It is important to identify and manage allergies effectively to reduce the production of thick phlegm and alleviate associated respiratory symptoms. Understanding the role of allergies in the development of excessive mucus production is crucial in implementing appropriate prevention and treatment strategies.
Exploring the Association Between Smoking and Excessive Mucus Buildup
When it comes to the connection between smoking and the accumulation of excessive mucus in the respiratory system, it is essential to delve further into the intricate relationship that exists. By examining the effects of smoking on the body, particularly on the respiratory system, we can gain a better understanding of how smoking can contribute to the production of thick phlegm, often leading to discomfort and potential health issues.
In numerous studies, scientists have observed an undeniable correlation between smoking and the increase in mucus production within the respiratory tract. Long-term smoking can irritate the airways and cause inflammation, leading to excessive production and thickening of mucus. This thickened mucus can become trapped within the air passages, making it difficult to expel, and commonly leading to symptoms such as coughing, wheezing, and chest congestion.
Moreover, the harmful chemicals present in tobacco smoke can damage the cilia - the hair-like structures responsible for sweeping mucus out of the respiratory system. As a result, the impaired cilia are less effective in removing mucus, further contributing to the accumulation of thick phlegm in the airways.
Apart from the immediate effects on mucus production, smoking also poses a long-term risk. The continuous exposure to cigarette smoke can lead to chronic bronchitis, a condition characterized by persistent inflammation of the airways. In chronic bronchitis, excessive mucus production and the associated cough become a chronic issue, impacting the individual's quality of life and increasing the risk of developing more severe respiratory diseases.
While quitting smoking is the most effective way to alleviate the symptoms and prevent further complications associated with excessive mucus buildup, there are also some remedies that can provide temporary relief. Drinking plenty of fluids, using a humidifier, and practicing healthy lifestyle habits such as regular exercise and a balanced diet can help in thinning mucus and promoting its elimination from the respiratory system.
In conclusion, understanding the link between smoking and the production of thick phlegm is crucial for individuals who may experience respiratory discomfort. By recognizing the effects of smoking on mucus production and taking steps towards smoking cessation and adopting healthy habits, individuals can improve their respiratory health and reduce the burden of excessive mucus buildup.
The Role of Infections in the Formation of Thick Mucus
In the context of discussing the factors contributing to the development of viscous and dense mucus, it is crucial to emphasize the significant role that infections play in this process. Infections can exert a profound influence on the consistency and texture of mucus, leading to the production of thick and sticky phlegm. Understanding the connection between infections and the formation of dense mucus is essential in comprehending the underlying mechanisms and in exploring potential remedies for this condition.
Infections: Whenever the body is exposed to harmful bacteria, viruses, or other pathogens, the immune system responds by triggering an inflammatory response. This immune response typically leads to the activation of various immune cells and the release of inflammatory mediators. In the context of mucus production, infections can directly affect the glands responsible for producing mucus, leading to an increased secretion of thick and sticky phlegm.
The Impact of Inflammatory Mediators: In the presence of infections, inflammatory mediators, such as cytokines and chemokines, are released. These molecules serve as signaling molecules within the body, orchestrating the immune response. They contribute to the recruitment and activation of immune cells in the affected area, which, in turn, leads to an increased production of mucus. Additionally, the presence of inflammatory mediators can alter the composition and properties of mucus, making it more viscous and difficult to clear.
Mucociliary Clearance Impairment: Infections can also impair the normal functioning of the cilia lining the respiratory tract. Cilia are tiny hair-like structures that help in moving mucus and trapped particles out of the lungs. When inflamed or damaged by infections, the cilia's effectiveness may be reduced, resulting in a slower clearance of mucus. This slower clearance, coupled with the increased production of thick mucus, can contribute to the accumulation of phlegm in the airways.
Conclusion: Infections play a crucial role in the creation of thick and sticky phlegm. The immune response triggered by infections leads to increased mucus production, alterations in mucus properties, and impairment of mucociliary clearance. By understanding the relationship between infections and mucus consistency, healthcare professionals can develop effective strategies to manage and alleviate the symptoms associated with this condition.
Lifestyle Changes for Reducing Excessive Mucus Production
When it comes to managing the overproduction of thick mucus, making certain changes to one's daily habits and lifestyle can significantly contribute to improving overall respiratory health. By incorporating these lifestyle modifications, individuals can potentially reduce the excessive build-up of sticky, viscous phlegm.
First and foremost, it is essential to prioritize hydration. Ensuring that you are adequately hydrated by drinking plenty of fluids, such as water and herbal teas, can help thin out mucus and make it easier to expectorate. Additionally, avoiding dehydrating beverages like alcohol and caffeine is advised, as they can contribute to the thickening of mucus.
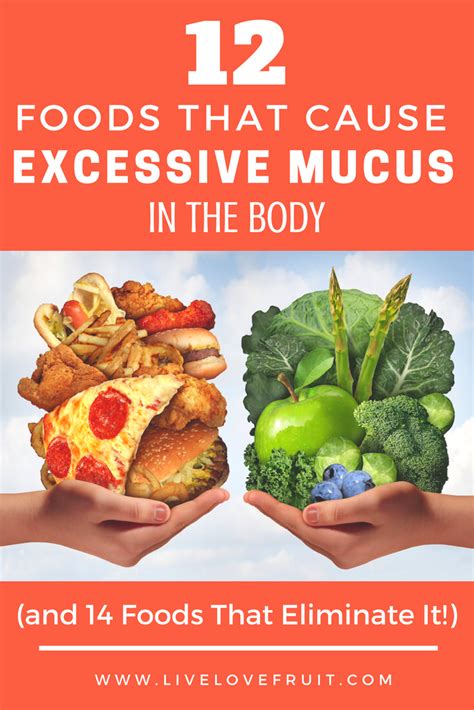
Another lifestyle change that can be beneficial in reducing mucus production is maintaining a healthy diet. Consuming a well-balanced diet rich in fruits, vegetables, and whole grains provides the body with essential nutrients to support healthy respiratory function. Avoiding processed foods, refined sugars, and excessive dairy consumption can help reduce inflammation and congestion in the airways, ultimately lessening the production of thick phlegm.
| Essential Lifestyle Changes to Reduce Thick Phlegm | |
|---|---|
| Stay hydrated by drinking plenty of water and herbal teas. | ✔ |
| Avoid dehydrating beverages like alcohol and caffeine. | ✔ |
| Follow a well-balanced diet rich in fruits, vegetables, and whole grains. | ✔ |
| Avoid processed foods, refined sugars, and excessive dairy consumption. | ✔ |
| Engage in regular physical exercise to promote respiratory health. | ✔ |
| Maintain a clean and dust-free environment to minimize allergens. | ✔ |
Regular physical exercise can also play a crucial role in reducing the production of thick mucus. Engaging in activities that promote cardiovascular health can help improve circulation and enhance lung function. Additionally, exercise can stimulate the body's natural ability to clear mucus from the airways, assisting in its expulsion.
Lastly, creating and maintaining a clean and dust-free environment is essential in minimizing allergens that can trigger excessive mucus production. Regularly cleaning surfaces, using air purifiers, and keeping indoor humidity levels in check can help reduce respiratory irritants and decrease the chances of experiencing thick, sticky phlegm.
By embracing these lifestyle changes and incorporating them into your daily routine, you can take proactive steps towards reducing the production of excessive, thick mucus. However, it is always important to consult with a healthcare professional if the symptoms persist or worsen.
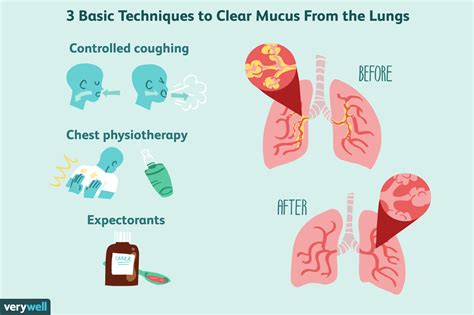
Natural Ways to Help Clear Thick Mucus
In this section, we will explore various natural remedies that can aid in alleviating the discomfort caused by excessive phlegm. By incorporating these remedies into your daily routine, you may be able to effectively promote the removal and thinning of dense mucus.
- Stay Hydrated: Drinking plenty of fluids, such as water and herbal teas, can help hydrate your body and thin out the thick mucus, making it easier to expel.
- Steam Inhalation: Inhaling steam generated from a hot shower or a bowl of hot water with essential oils can help loosen the phlegm, providing relief and assisting in its removal.
- Saltwater Gargles: Gargling with warm saltwater can effectively soothe irritated throat tissues and aid in reducing the thickness of mucus in the throat.
- Eucalyptus Oil: Inhalation or topical application of eucalyptus oil can help clear congestion, as it contains properties that can break down thick mucus and provide respiratory relief.
- Ginger: Consuming ginger in various forms, such as ginger tea or adding it to your meals, can help promote mucus thinning and aid in its expulsion due to its natural expectorant properties.
- Honey and Lemon: A mixture of warm water, honey, and lemon juice can soothe the throat and help break down and clear the excess mucus.
- Warm Liquids: Drinking warm liquids, such as herbal teas, broths, or warm water with honey, can provide relief by thinning thick mucus.
- Humidifier: Using a humidifier or a vaporizer in your living environment can add moisture to the air and help prevent the thickening of mucus in the respiratory system.
- Healthy Diet: Consuming a well-balanced diet rich in fruits and vegetables can support your immune system and overall respiratory health, aiding in the reduction of thick phlegm.
- Regular Exercise: Engaging in regular physical activity can help improve circulation, promote airway clearance, and assist in the thinning of mucus, thus facilitating its expulsion.
By incorporating these natural remedies into your daily routine, you can take proactive steps towards clearing thick phlegm and experiencing relief from associated symptoms. It is important to consult with a healthcare professional if symptoms persist or worsen.
Seeking Medical Attention for Thick Phlegm Issues: When to Take Action
Knowing when to seek medical attention for concerns related to thick phlegm can be crucial in identifying and resolving potential underlying health issues. While there are various causes, symptoms, and remedies associated with this condition, it is important to understand when professional guidance is necessary.
Recognizing persistent symptoms
While occasional bouts of thick phlegm may not immediately warrant medical attention, persistent symptoms should not be overlooked. If you consistently experience difficulty breathing, a chronic cough, chest pain, or related respiratory issues, it is advisable to consult with a healthcare professional. They can help determine the root cause of your symptoms and suggest appropriate treatment options.
Monitoring changes in phlegm appearance and consistency
Changes in the appearance or consistency of phlegm may indicate an underlying health condition. If you notice sudden changes, such as an increase in thickness, color (such as green or yellow), or the presence of blood, it is crucial to seek medical attention promptly. These changes could be indicative of an infection or inflammation in the respiratory system, and a medical professional can provide the necessary evaluation and guidance.
Assessing impact on daily life
If thick phlegm is significantly impacting your daily activities, it is essential to reach out to a healthcare provider. Persistent coughing fits, throat discomfort, or difficulty speaking due to excess phlegm can affect your quality of life. Seeking medical attention can help address these issues and provide relief through appropriate interventions and management strategies.
Considering underlying health conditions
Individuals with pre-existing respiratory conditions, such as asthma or chronic bronchitis, should be especially vigilant when it comes to thick phlegm symptoms. If you notice a worsening of your condition, increased frequency of symptoms, or if your current treatments are not providing relief, it is crucial to consult with a healthcare professional. They can assess your specific situation and adjust your treatment plan accordingly.
Trusting your instincts
If you have concerns or a gut feeling that something is not right with your thick phlegm issue, it is always better to be safe than sorry. Trusting your instincts and reaching out to a medical professional can provide reassurance and peace of mind. They can evaluate your symptoms, identify potential causes, and recommend appropriate next steps to address the issue effectively.
It is important to remember that while the above guidelines can help you determine when to seek medical attention for thick phlegm issues, a healthcare professional is the best resource to provide personalized advice based on your specific circumstances.
FAQ
What are the potential causes of thick phlegm?
The potential causes of thick phlegm include respiratory infections, allergies, smoking, pollution, and certain medical conditions such as bronchitis or sinusitis.
What are the common symptoms of thick phlegm?
The common symptoms of thick phlegm include coughing, difficulty in breathing, chest congestion, post-nasal drip, sore throat, and a feeling of heaviness in the chest.
Are there any natural remedies to alleviate thick phlegm?
Yes, there are several natural remedies that can help alleviate thick phlegm. Drinking plenty of fluids, using a humidifier, inhaling steam, gargling with saltwater, and consuming foods like ginger, garlic, and honey can provide relief.
How long does it usually take for thick phlegm to go away?
The duration for thick phlegm to go away varies depending on the underlying cause and individual factors. In most cases, it resolves within a few days to a couple of weeks. However, if the symptoms persist or worsen, it is advisable to seek medical attention.
When should I see a doctor if I have thick phlegm?
You should consider seeing a doctor if you have persistent thick phlegm that lasts for more than two weeks, if the phlegm becomes bloody or discolored, if you experience high fever, chest pain, or difficulty in breathing, or if the symptoms significantly affect your daily life.
What causes the production of thick phlegm?
Thick phlegm can be caused by various factors, including respiratory infections such as colds and bronchitis, allergies, smoking, and exposure to pollutants.



