In our quest for radiant and flawless skin, we are often confronted with peculiar occurrences that may give rise to a multitude of questions. One such topic that continues to puzzle and intrigue is the emergence of colorless spots on our flesh. These enigmatic patches, devoid of pigmentation, can manifest on individuals of all ages and backgrounds, leaving many yearning for an understanding of their origin and potential treatments.
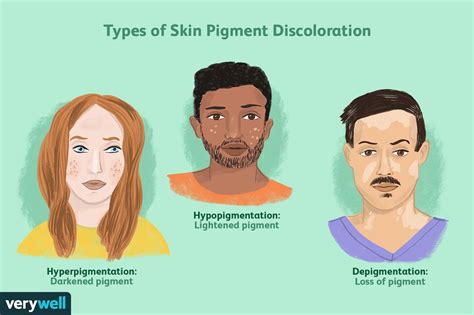
When our skin loses its characteristic hue, it presents a unique challenge to both the affected individual and medical professionals alike. Through observations and examinations, experts have recognized that the absence of melanin, the pigment responsible for coloration, gives rise to these intriguing and curious white blemishes. They can appear seemingly out of the blue, without warning or cause, leading to a relentless quest for answers and solutions.
Expressions of curiosity and concern often accompany the first appearance of these depigmented patches. Whether it is unabashedly noticeable or subtly concealed beneath layers of clothing, the impact on one's self-esteem can be profound. The ramifications extend beyond the tangible physicality, echoing into the realms of mental and emotional well-being. Naturally, individuals yearn for respite, a way to reclaim their confidence and reestablish a harmonious balance within their epidermis.
Vitiligo: The Most Prevalent Cause of Hypopigmentation

Vitiligo, an encompassing term for the most commonly observed skin disorder characterized by patches of hypo or depigmented skin, holds a significant position among the various etiologies responsible for white spots on the skin. Predominantly observed in both sexes and across different ethnicities, this dermatological condition affects a considerable portion of the global population, causing aesthetic concerns and occasionally impacting the quality of life for those affected.
Autoimmune Disorders: Connecting the Dots
In the realm of skin conditions characterized by white patches, there exists a group of disorders that are not solely concerned with the understanding, causes, and treatment of these patches. Instead, a deeper connection has been established, unveiling the intricate relationship between the body's immune system and the onset of these conditions. Referred to as autoimmune disorders, these conditions are marked by the immune system mistakenly attacking healthy cells and tissues, resulting in a myriad of symptoms that extend far beyond the physical appearance of white patches on the skin.
Drawing a definitive link between autoimmune disorders and white patches, it becomes evident that the underlying mechanisms at play are far more complex than previously understood. While the understanding of these conditions is still evolving, current research suggests that autoimmune disorders can manifest differently in different individuals, leading to a wide range of symptoms, including skin discoloration. By connecting the dots between these two seemingly unrelated phenomena, medical experts and researchers are beginning to shed light on the intricate web of interactions taking place within the body.
Autoimmune disorders are not limited to the skin alone - they can affect various organs and systems throughout the body. By exploring the common threads among different autoimmune disorders, scientists are unveiling shared genetic and environmental factors that contribute to their development. Understanding these connections is crucial in unraveling the underlying causes of white patches on the skin and developing targeted treatments that address the root cause rather than focusing solely on managing the visible symptoms.
While treatment options for autoimmune disorders are available, they often focus on suppressing the immune system to alleviate symptoms. However, the current direction of research emphasizes the need for personalized approaches that tackle the specific mechanisms contributing to each individual's autoimmune disorder. By uncovering the underlying causes and triggers, medical professionals aim to develop targeted therapies that not only manage the visible manifestation of white patches but also modulate the immune response to halt the progression and minimize the impact of autoimmune disorders on overall health.
Genetic Factors: Is Your DNA Responsible for Skin Discoloration?
Many individuals with patches of discoloration on their skin have wondered about the role of genetic factors in this phenomenon. While it is commonly known that external factors such as sun exposure and certain medical conditions can contribute to the appearance of white patches, the influence of one's DNA on the development of skin discoloration remains a topic of interest and ongoing research.
Researchers have been investigating whether certain genes and genetic variations are associated with an increased risk of developing white patches on the skin. These studies aim to unravel the intricate relationship between an individual's genetic makeup and the manifestation of skin pigmentation abnormalities, providing a deeper understanding of the underlying causes.
Although specific genes responsible for pigmentation disorders are yet to be fully identified, scientists have made significant progress in identifying potential genetic markers and variations that could be associated with the development of white patches. These findings have the potential to provide new insights into the mechanisms behind the loss of melanocytes, the pigment-producing cells, leading to depigmentation.
Genetic factors may also play a role in determining the severity and progression of pigmentation disorders. Some individuals may be more susceptible to developing extensive depigmentation due to specific genetic variations, while others may experience milder forms of discoloration. Understanding these genetic predispositions could pave the way for tailored treatment strategies and interventions.
While it is important to acknowledge the influence of genetic factors, it is crucial to remember that not everyone with a predisposition to certain gene variants will develop white patches on their skin. Environmental factors and other triggers can still contribute significantly to the manifestation of discoloration. Researchers continue their efforts to unravel the complex interplay between genes, environmental influences, and the appearance of white patches on the skin.
Photochemotherapy: A Promising Treatment Option
In the realm of understanding the underlying factors and effective solutions for the occurrence of light-colored patches on the surface of the skin, photochemotherapy has emerged as a promising treatment approach. This innovative therapeutic method harnesses the powerful combination of light and medication to target and alleviate the symptoms associated with depigmentation.
Refining the healing power of light:
Photochemotherapy, also known as psoralen plus ultraviolet A (PUVA) therapy, involves the administration of a photosensitizing medication followed by exposure to UVA light. Through a carefully controlled process, this treatment method stimulates repigmentation of the affected areas, offering hope for individuals seeking an effective solution for white patches on their skin.
Enhancing melanin production:
The combination of photosensitizing medication and UVA light activates the melanocytes, which are responsible for producing melanin, the pigment that gives color to the skin, hair, and eyes. By targeting these key cells and encouraging melanin production, photochemotherapy aims to restore the natural pigmentation to the lightened areas, thus diminishing the appearance of white patches.
Targeting specific affected areas:
A significant advantage of photochemotherapy is its ability to selectively target the affected areas without affecting the surrounding healthy skin. By focusing the UVA light on the depigmented patches, this treatment option minimizes the risk of adverse effects on unaffected skin, providing a safe and localized approach to depigmentation treatment.
Monitoring progress and adjusting treatment:
Throughout the photochemotherapy process, regular monitoring and evaluation of the patient's progress are essential. By closely observing the skin's response to the treatment, healthcare professionals can make necessary adjustments to the dosage of medication and light exposure, tailoring the therapy to each individual's needs and maximizing its effectiveness.
In conclusion, photochemotherapy emerges as a promising option for individuals seeking viable solutions for white patches on their skin. By combining medication and targeted UVA light exposure, this treatment method aims to stimulate melanin production and restore natural skin pigmentation, offering a potential remedy for those affected by depigmentation.
The Impact of Stress on the Formation of Hypopigmentation
As the development of white patches on the skin continues to raise questions, researchers have turned their attention to the role of stress in this phenomenon. Stress, a multifaceted psychological and physiological response provoked by various external and internal factors, has been found to potentially contribute to the formation of hypopigmentation, commonly known as white patches on the skin.
While the exact mechanisms behind how stress triggers the formation of white patches remain elusive, numerous studies have suggested a strong correlation between stress and the disruption of melanin production. Melanin, the pigment responsible for giving color to the skin, hair, and eyes, plays a crucial role in protecting the skin from harmful UV radiation. When stress levels are elevated, certain chemicals and hormones released by the body may interfere with the normal functioning of melanocytes, the melanin-producing cells, leading to a decrease in melanin production. Furthermore, stress-induced immune system dysregulation has been implicated in the development of white patches on the skin. Stress can alter immune responses, potentially triggering autoimmune reactions that target melanocytes. This autoimmune response can result in the destruction of melanocytes, leading to the appearance of white patches. Moreover, psychological stress can manifest in self-destructive behaviors such as excessive scratching or rubbing of the skin, which can physically damage melanocytes or disturb their functioning. The repeated trauma on the skin can disrupt melanin production and contribute to the formation of white patches. |
Melanocyte Destruction: What Happens to the Pigment Cells?
Understanding the underlying mechanisms behind white patches on the skin involves delving into the fascinating world of melanocytes. These pigmented cells play a crucial role in determining the color of our skin, hair, and eyes. However, when melanocytes encounter destruction, the consequences can lead to the development of white patches, known as hypopigmentation or depigmentation.
Melanocyte destruction refers to the damage or loss of melanocytes, which are responsible for producing melanin, the pigment that gives color to the skin. This can occur due to various factors such as autoimmune disorders, genetic conditions, sun damage, or certain skin diseases. When melanocytes are affected, the production of melanin is disrupted, resulting in the formation of white patches on the skin.
What happens to the pigment cells? When melanocytes are destroyed, it leads to a decrease in the production of melanin, causing a localized loss of color in the affected areas. The mechanism behind melanocyte destruction varies depending on the underlying cause. In some cases, the immune system mistakenly targets and attacks melanocytes, leading to their destruction. In others, genetic factors or external factors like UV radiation contribute to the damage of these cells.
Autoimmune disorders such as vitiligo involve the immune system mistakenly recognizing melanocytes as foreign invaders and launching an attack against them. This immune response results in the destruction of melanocytes and subsequent loss of pigmentation. Similarly, certain genetic conditions can lead to abnormal melanocyte function or increased susceptibility to damage, ultimately resulting in the development of white patches on the skin.
Excessive sun exposure can also play a role in melanocyte destruction. Ultraviolet (UV) radiation from the sun damages melanocytes and impairs their ability to produce melanin. Over time, this can lead to the development of hypopigmentation or the formation of white patches on sun-exposed areas of the skin.
Understanding the process of melanocyte destruction is crucial for developing effective treatments and interventions. By unraveling the intricacies of what happens to these pigment cells, researchers and healthcare professionals can work towards developing strategies to prevent or reverse their destruction, ultimately leading to improved management of white patches on the skin.
Natural Remedies: Exploring Alternative Treatment Approaches

In this section, we will delve into alternative methods for addressing and managing those pale spots that can appear on the surface of our bodies. While it is essential to comprehend the origins and cures of these discolorations, investigating the potential of natural remedies can offer additional options in our quest for a solution.
When seeking alternative ways to tackle these particular conditions, it is crucial to explore unconventional methods that go beyond mainstream treatments. While conventional treatments focus on medical interventions, natural remedies embrace a more holistic approach, leveraging the power of nature to aid in the healing process.
One fascinating avenue to consider in the realm of natural remedies is the utilization of herbal extracts, which have been used for centuries in traditional medicine. These extracts, known for their therapeutic properties, can potentially promote the rejuvenation of the skin, thereby reducing the appearance of white patches.
Furthermore, exploring the potential benefits of essential oils could unveil promising options for those seeking alternative treatments. Certain essential oils possess properties that can aid in cell regeneration, restoring the skin's natural pigmentation and reducing the contrast between pale and unaffected areas.
Additionally, incorporating specific dietary changes and supplements into our daily routines may also prove beneficial in combating these patches. By focusing on consuming a well-balanced diet rich in essential nutrients, vitamins, and minerals, we can aim to support our body's healing mechanisms and potentially reduce the visibility of white spots.
It is important to note that while natural remedies can offer alternative treatment approaches, it is essential to consult with a healthcare professional before embarking on any new treatment regimen. Each individual's circumstances and needs are unique, and professional guidance ensures the most appropriate and effective approach to addressing these skin conditions.
Exploring the realm of natural remedies allows us to broaden our perspective on addressing white patches on the skin beyond conventional medical treatments. By embracing alternative approaches that harness the power of nature, we may discover compelling avenues for rejuvenation and healing.
Coping with Social Stigma: Support and Awareness Matters
Addressing the social challenges associated with the appearance of light-colored patches on the skin requires understanding the impact of these markings beyond their physical manifestations. This section focuses on the ways individuals can cope with social stigma by seeking support and promoting awareness.
Seeking Support and Understanding:
Dealing with the stares, comments, or misconceptions from others can be emotionally overwhelming for individuals affected by discoloration on their skin. It is crucial to seek support from friends, family, or professional counselors who can provide empathy, encouragement, and understanding. Engaging in open discussions about the emotional impact of social stigma can help alleviate feelings of isolation and build resilience.
Raising Awareness:
Generating awareness about the underlying causes of these skin patches and debunking common myths is essential in combating social stigma. By educating communities and promoting accurate information, individuals can help challenge stereotypes and promote a more inclusive and empathetic society. This can be achieved through participating in awareness campaigns, organizing educational events, and sharing personal experiences through various mediums.
Building Confidence:
Developing a strong sense of self-esteem and self-acceptance is key to overcoming the negative impact of social stigma. Embracing one's unique features and learning to love oneself can empower individuals to embrace their appearance and resist any external pressures or judgments. Engaging in activities that promote self-care, such as practicing self-affirmations, seeking therapeutic activities, or joining support groups, can contribute to building confidence and fostering a positive self-image.
Supporting Others:
Showing support and understanding to those affected by skin discoloration can make a significant difference in their lives. By demonstrating empathy, avoiding judgment, and challenging discriminatory behavior, individuals can contribute to creating a more compassionate and inclusive environment. Encouraging others to educate themselves and fostering empathy can further minimize the impact of social stigma and promote a more accepting society.
FAQ
What are the causes of white patches on the skin?
White patches on the skin can be caused by various factors. One common cause is a condition called vitiligo, which occurs when the cells that produce melanin, the pigment that gives color to the skin, stop functioning. Other possible causes include fungal infections, autoimmune diseases, and genetic factors.
Can white patches on the skin be treated?
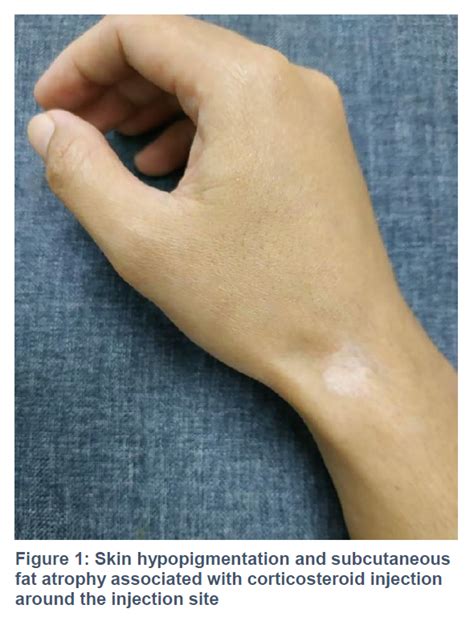
Yes, there are treatment options available for white patches on the skin. The choice of treatment depends on the underlying cause. In the case of vitiligo, treatment options may include topical corticosteroids, topical immunosuppressants, or light therapy. For fungal infections, antifungal medications may be prescribed. It is important to consult a dermatologist for an accurate diagnosis and appropriate treatment.
Are white patches on the skin contagious?
No, white patches on the skin are not contagious. Most conditions that cause white patches, such as vitiligo, are not contagious or caused by any infectious agent. These conditions are primarily due to problems with pigmentation or autoimmune responses in the body. It is important to understand that these patches do not pose any risk of spreading to others.
Can white patches on the skin be prevented?
While it may not be possible to prevent all cases of white patches on the skin, there are some steps that can be taken to minimize the risk. Protecting the skin from excessive sun exposure by using sunscreen and wearing protective clothing can help reduce the chances of developing certain conditions that can cause white patches, such as vitiligo. Additionally, maintaining a healthy lifestyle and managing stress levels may also contribute to overall skin health.



